The osteoarthritis of the hip joint (deforming osteoarthritis, coxarthrosis, osteoarthrosis) is a slowly progressive degenerative-district disease, which takes over time to destroy the affected joint, persistent pain and limiting mobility.
The disease affects people over 40, women get sick several times more often than men.
In the general structure of osteoarthritis, the osteoarthritis of the hip joint belongs to the main role.This is due to the generalized congenital pathology of the hip joints (dysplasia), as well as a significant physical effort, to which these joints are susceptible.
Risk factors and causes of osteoarthritis of the hip joint
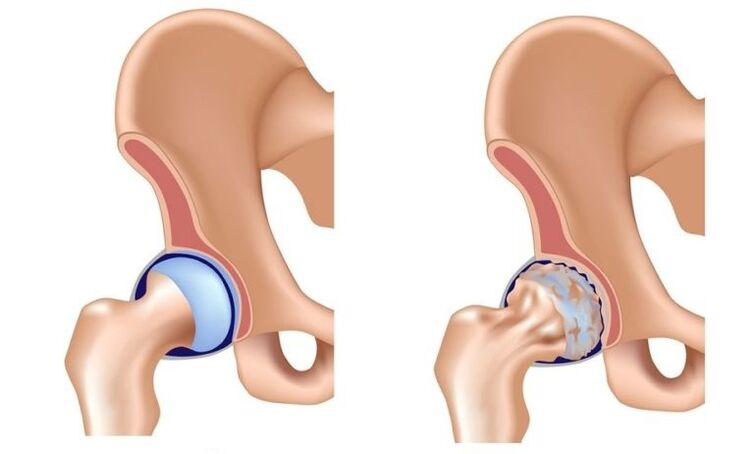
In the pathological mechanism of the development of the osteoarthritis of the hip joint, the main role belongs to a change in the physicochemical characteristics of the synovial (intra -articular) fluid, as a result of which it becomes denser and more viscous.This worsens its lubricating qualities.When it moves, the cartilage surfaces of the joint begin to rub each other, they become rough, cracks.Small hyaline cartilage particles are abandoned and fall into joint cavity, which causes the development of aseptic inflammation (not infectious).As the disease progresses to the inflammatory process, bone tissue is introduced into the inflammatory process, which leads to aseptic necrosis of the femoral head sections and the surface of the acetabulum, the formation of osteophytes (bone growth), improvement of inflammation and causes severe pain during the movement.
In the late extension of the osteoarthritis of the hip joint, the inflammation is also thrown into the surrounding joint of the tissue (blood vessels, nerves, ligaments, muscles), which leads to the appearance of signs of periartritis.As a result, the hip joint is completely destroyed, its functions are lost, the movement in it ceases.This condition is called anquilosis.
Causes of osteoarthritis of the hip joint:
- Congenital lip of thighs;
- hip dysplasia;
- Aseptic necrosis of the femoral head;
- Peters disease;
- Hip joint injuries;
- infectious arthritis of the hip joint;
- gonarrosis (deforming osteoarthrosis of the knee joint);
- osteochondrosis;
- Overweight;
- professional sports;
- flat feet;
- spine curvature;
- A sedentary lifestyle.
The pathology is not inherited, but the child inherits the characteristics of the structure of the musculoskeletal system of their parents, which can cause osteoarthritis of the hip joint under these conditions.This explains the fact of the existence of families, whose incidence is higher than in the general population.
Disease forms
Depending on the etiology, the osteoarthritis of the hip joint is divided into primary and secondary.Secondary osteoarthritis is developed in the context of other hip joint diseases or its injuries.The main form is not related to the previous pathology, the reason for its development is often not possible, in this case they speak of idiopathic osteoarthritis.
Cooksarrosis is one or bilateral.
Stages
Three stages (grade) are distinguished during the osteoarthritis of the hip joint:
- Pathological initial changes are expressed slightly, provided that timely and adequate treatment is reversible.
- Progressive coxarthrosis: characterized by a gradual increase in symptoms (articulation pain and deteriorated their mobility), changes in joint tissues are already irreversible, but therapy can slow down the degenerative processes.
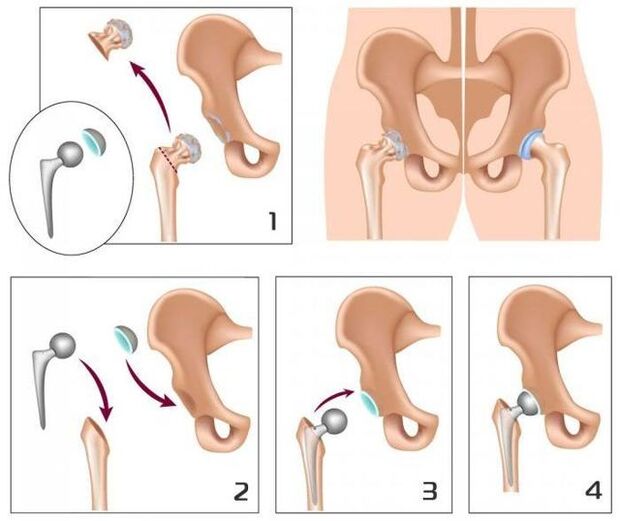
- The final movement in the joint is lost, anquilosis is formed.The treatment is only surgically (replacing the artificial joint).
Endoprotic operations in 95% of cases ensure a complete restoration of limb mobility, restore patient performance.

Symptoms of the arthrohrosis of the hip joint
The main signs of osteoarthritis of the hip joint:
- Pain in groin, hips and knees;
- a sensation of stiffness in the affected joint and the limitation of its mobility;
- limp;
- abduction restriction;
- Atrophic changes in the muscles of the thigh.
The presence of certain symptoms of osteoarthritis of the hip joint, as well as its severity depends on the degree of disease.
In the first degree of osteoarthritis of the hip joint, patients complain about the pain in the affected joint that occurs under the influence of physical activity (prolonged walk, race).In some cases, the pain is located in the area of the knee or thigh.After a short break, the pain passes on its own.The volume of limb movements is completely preserved, the march is not broken.The following changes are observed in the radiography:
- slight unequal decrease in the light of the joint gap;
- Osteophytes located on the inner edge of the turn.
No changes of the neck and femoral head are detected.
With the II degree of osteoarthritis of the hip joint, pain also appears at rest, even at night.After physical activity, the patient begins to limit, a characteristic "duck" is formed.Then, start pains appear called: After a long period of immobility, the first steps cause pain and discomfort, which then pass and then return after a long load.In the affected joint, the volume of movements (abduction, internal rotation) is limited.The radiography shows that the joint gap is reduced unequally and its light is 50% of the standard.Osteophytes are found along the internal and external edge of the joint cavity, going beyond the limits of the cartilage.The contours of the femoral head become unequal due to the deformation.
With the III Degree of osteoarthritis of the articulation of the hip of pain, intense and constant, without stopping at night.Walking is significantly difficult, the patient is forced to trust the cane.The volume of movements in the affected joint is very limited, then stops completely.Due to the atrophy of the hip muscles, the pelvis deviates in the frontal plane and the limb is shortened.When trying to compensate for this shortening, patients when walking are forced to reject the body towards the lesion, which further increases the load in the sore joint.In radiographs, multiple bone growths are detected, significant narrowing of the joint gap and a pronounced increase in the head of the femur.
Diagnosis
The diagnosis of osteoarthritis of the hip joint is based on data on the clinical image of the disease, the results of the medical examination and instrumental studies, among which the main value belongs to the visualization methods: radiography, calculated or magnetic resonance images.They allow not only to determine the presence of osteoarthritis of the hip joint and evaluate its degree, but also to identify the possible cause of the disease (trauma, youth epifisonisis, Peters disease).
The differential diagnosis of the osteoarthritis of the hip joint with other diseases of the musculoskeletal system is quite complicated.In the degree of osteoarthritis II and III of the hip joint, muscle atrophy develops, which can cause intensive pain in the knee joint characteristic of impulse or gonarrosis (knee joint diseases).For the differential diagnosis of these states, the palpation of the knee joints and the hip is palpated, the volume of movement is determined in them and are also examined by radiologically.
In column diseases, in some cases, the nerve roots of the spinal cord with the development of pain syndrome are squeezed.The pain can radiate to the area of the hip joint and imitate the clinical picture of its defeat.However, the nature of pain with root syndrome is slightly different from the osteoarthritis of the hip joint:
- Pain occurs as a result of weightlifting or an acute awkward movement, and not under the influence of physical effort;
- The pain is located in the buttock, not in the inguinal region.
With the root syndrome, the patient can calmly carry the leg aside, while with the osteoarthritis of the hip joint, the kidnapping is limited.A characteristic sign of root syndrome is a positive tension symptom: the appearance of acute pain when trying to lift a straight leg on the patient's back.
Hip joint osteoarthritis affects people over 40, women get sick several times more often than men.
The osteoarthritis of the hip joint should also be differentiated with loyal bursite (trocontitis).Student bursitis develops faster, in a few weeks.It is usually preceded by significant physical effort or injuries.In this disease, pain is much more pronounced than with the osteoarthritis of the hip joint.At the same time, it is not detected to shorten the limb and limit its mobility.
The clinical picture of atypical reactive arthritis and ankylosing spondylitis may resemble the clinical manifestations of the arthrosis of the hip joint.However, pain occurs in patients mainly at night or at rest, when walking does not intensify, but, on the contrary, it weakens.In the morning, patients indicate stiffness in the joints, which passes after a few hours.
Treatment of hip joint osteoarthritis
Orthopedic are dedicated to the treatment of the osteoarthritis of the hip joints.With the degree of disease I and II, conservative therapy is indicated.With pronounced pain syndrome, patients receive non -steroid anti -inflammatory medications in a short course.They should not be accepted for a long time, since they can not only have a negative effect on the organs of the gastrointestinal tract, but also suppress the regenerative skills of the Hyalin cartilage.
In the treatment regime of the articulation of the hip, they include condroprotectors and vasodilators, which creates optimal opportunities to restore damaged cartilage tissues.With pronounced muscle spasm, the appointment of central muscle relaxants may require.
In those cases where it is not possible to stop pain with non -steroid anti -inflammatory drugs, they resort to intra -articular corticosteroid injections.
The local treatment of the arthrosis of the hip joint using ointments in heating allows you to reduce muscle spasm and weaken some pain due to the distraction action.
In the complex therapy of the arthrosis of the hip joint, physiotherapeutic methods are also used:
- Magnetotherapy;
- inductothermia;
- UHF;
- laser therapy;
- ultrasound treatment;
- massage;
- Medical Gymnastics;
- Manual therapy
Dietary nutrition for the osteoarthritis of the hip joint aims to correct body weight and normalization of metabolic processes.Reducing body weight reduces load in hip joints and, therefore, slows down the progression of the disease.
To download the affected joint, the doctor may recommend that patients go to the crutches or the cane.
With the degree III of osteoarthritis of the hip joint, conservative treatment is inefficient.In this case, it is possible to improve the condition of the patient, it is possible to return normal mobility only as a result of surgical intervention, replacing the artificial articulation (artificial endoprostic).
Possible consequences and complications
The most serious complication of the progressive osteoarthritis of the hip joint is disability due to the loss of movement in the joint.With bilateral cookarrosis, the patient loses his ability to move independently and needs constant strange attention.A long stay in bed in a position creates the previous requirements for the appearance of stagnant (hypostatic) pneumonia, which is difficult to succumb and can cause death.
The pathology is not inherited, but the child inherits the characteristics of the structure of the musculoskeletal system of his parents, which can cause osteoarthritis of the hip joint.
Forecast
The osteoarthritis of the hip joints is a progressive chronic disease, which can be completely cured only in the early stages, subject to the elimination of the cause of the disease.In other cases, the therapy allows you to slow down your course, however, over time, there is a need to implement hip endoprothesis.These operations in 95% of cases provide a complete restoration of limb mobility, restore patient performance.The useful life of modern prostheses is 15-20 years, after which they are subject to replacement.
Prevention
The prevention of the arthrosis of the hip joint aims to eliminate the causes that can lead to the development of this disease and includes:
- timely detection and treatment of diseases and hip joint injuries;
- rejection of a sedentary lifestyle, regular physical activity, but not excessive;
- body weight control;
- rational nutrition;
- Rejection of bad habits.

























